Abstract
Background and study aims
Accurate endoscopic detection of dysplasia in patients with Barrett’s esophagus (BE) remains a major clinical challenge. The current standard is to take multiple biopsies under endoscopic image guidance, but this leaves the majority of the tissue unsampled, leading to significant risk of missing dysplasia. Furthermore, determining whether there is submucosal invasion is essential for proper staging. Hence, there is a clinical need for a rapid in vivo wide-field imaging method to identify dysplasia in BE, with the capability of imaging beyond the mucosal layer. We conducted an ex vivofeasibility study using photoacoustic imaging (PAI) in patients undergoing endoscopic mucosal resection (EMR) for known dysplasia. The objective was to characterize the esophageal microvascular pattern, with the long-term goal of performing in vivo endoscopic PAI for dysplasia detection and therapeutic guidance.
Materials and methods
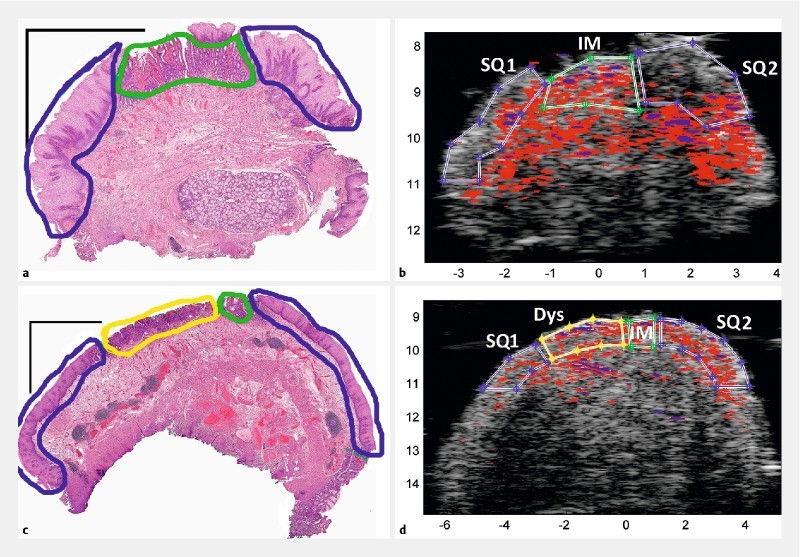
EMR tissues were mounted luminal side up. The tissues were scanned over a field of view of 14 mm (width) by 15 mm (depth) at 680, 750, and 850 nm (40 MHz acoustic central frequency). Ultrasound and photoacoustic images were simultaneously acquired. Tissues were then sliced and fixed in formalin for histopathology with hematoxylin and eosin staining. A total of 13 EMR specimens from eight patients were included in the analysis, which consisted of co-registration of the photoacoustic images with corresponding pathologist-classified histological images. We conducted mean difference test of the total hemoglobin distribution between tissue classes.
Results
Dysplastic and nondysplastic BE can be distinguished from squamous tissue in 84 % of region-of-interest comparisons (42/50). However, the ability of intrinsic PAI to distinguish dysplasia from NDBE, which is the clinically important challenge, was only about 33 % (10/30).
Conclusion
We demonstrated the technical feasibility of this approach. Based on our ex vivo data, changes in total hemoglobin content from intrinsic PAI (i. e. without exogenous contrast) can differentiate BE from squamous esophageal mucosa. However, most likely intrinsic PAI is unable to differentiate dysplastic from nondysplastic BE with adequate sensitivity for clinical translation.
