DaCosta RS, Kulbatski I, Lindvere-Teene L, Starr D, Blackmore K, Silver JI, Opoku J, Wu YC, Medeiros PJ, Xu W, Xu L, Wilson BC, Rosen C, Linden R; PLoS ONE 10(3): e0116623
doi.org/10.1371/journal.pone.0116623
Abstract
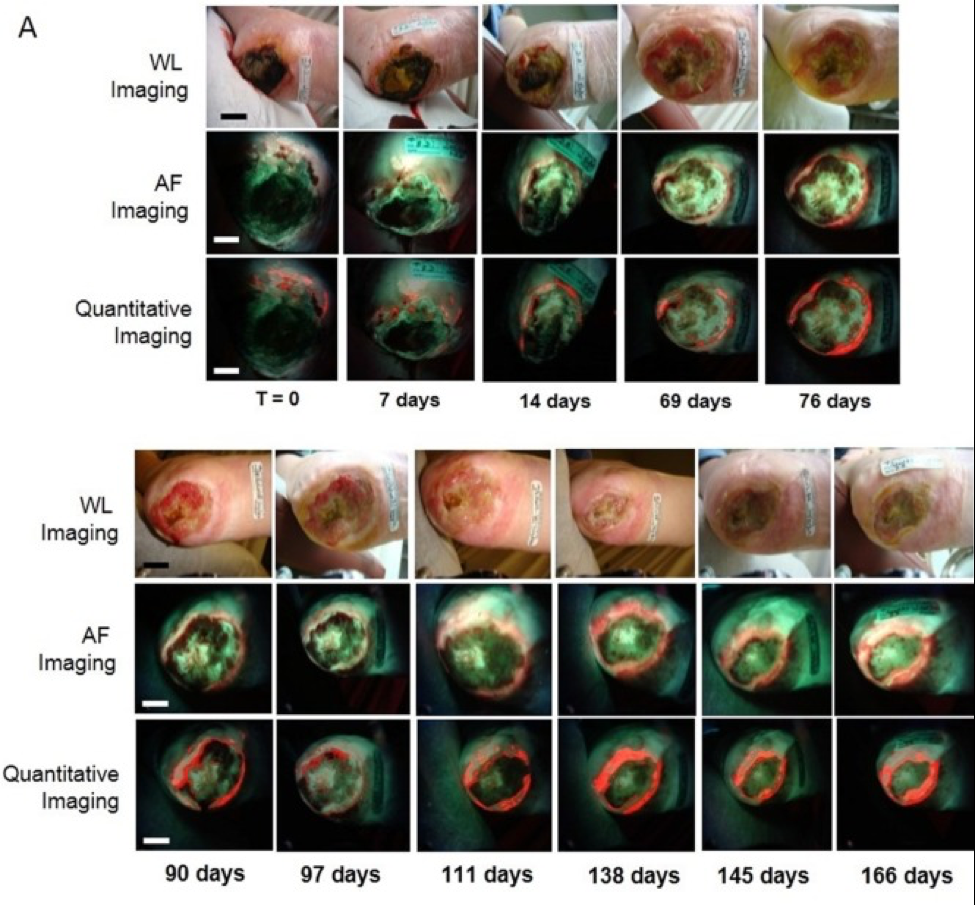
Traditionally, chronic wound infection is diagnosed by visual inspection under white light and microbiological sampling, which are subjective and suboptimal, respectively, thereby delaying diagnosis and treatment. To address this, we developed a novel handheld, fluorescence imaging device (PRODIGI) that enables non-contact, real-time, high-resolution visualization and differentiation of key pathogenic bacteria through their endogenous autofluorescence, as well as connective tissues in wounds. We designed a two-part Phase I, single center, non-randomized trial of chronic wound patients (male and female, ≥18 years; UHN REB #09-0015-A for part 1; UHN REB #12-5003 for part 2; clinicaltrials.gov Identifier: NCT01378728 for part 1 and NCT01651845 for part 2). Part 1 (28 patients; 54% diabetic foot ulcers, 46% non-diabetic wounds) established the feasibility of autofluorescence imaging to accurately guide wound sampling, validated against blinded, gold standard swab-based microbiology. Part 2 (12 patients; 83.3% diabetic foot ulcers, 16.7% non-diabetic wounds) established the feasibility of autofluorescence imaging to guide wound treatment and quantitatively assess treatment response. We showed that PRODIGI can be used to guide and improve microbiological sampling and debridement of wounds in situ, enabling diagnosis, treatment guidance and response assessment in patients with chronic wounds. PRODIGI is safe, easy to use and integrates into the clinical workflow. Clinically significant bacterial burden can be detected in seconds, quantitatively tracked over days-to-months and their biodistribution mapped within the wound bed, periphery, and other remote areas. In conclusion, PRODIGI represents a technological advancement in wound sampling and treatment guidance for clinical wound care at the point-of-care.