Ottolino-Perry K, Chamma E, Blackmore KM, Lindvere-Teene L, Starr D, Tapang K, Rosen CF, Pitcher B, Panzarella T, Linden R, DaCosta RS; Int Wound J. 2017 Oct;14(5):833-841
doi: 10.1111/iwj.12717
Abstract
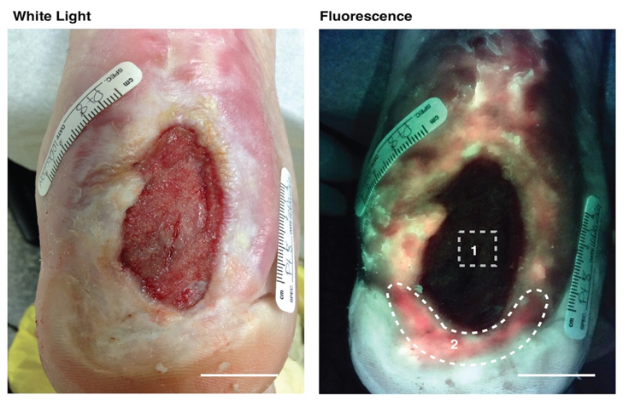
Clinical wound assessment involves microbiological swabbing of wounds to identify and quantify bacterial species, and to determine microbial susceptibility to antibiotics. The Levine swabbing technique may be suboptimal because it samples only the wound bed, missing other diagnostically relevant areas of the wound, which may contain clinically significant bacteria. Thus, there is a clinical need to improve the reliability of microbiological wound sampling. To address this, a handheld portable autofluorescence (AF) imaging device that detects bacteria in real time, without contrast agents, was developed. Here, we report the results of a clinical study evaluating the use of real-time AF imaging to visualise bacteria in and around the wound bed and to guide swabbing during the clinical assessment of diabetic foot ulcers, compared with the Levine technique. We investigated 33 diabetic foot ulcers (n = 31 patients) and found that AF imaging more accurately identified the presence of moderate and/or heavy bacterial load compared with the Levine technique (accuracy 78% versus 52%, P = 0·048; adjusted diagnostic odds ratio 7·67, P < 0·00022 versus 3·07, P = 0·066) and maximised the effectiveness of bacterial load sampling, with no significant impact on clinical workflow. AF imaging may help clinicians better identify the wound areas with clinically significant bacteria, and maximise sampling of treatment-relevant pathogens.